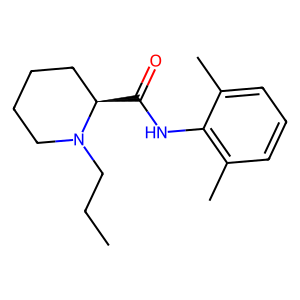
Ropivacaine powder is a local anesthetic medication that belongs to the amino amide group. It works by blocking nerve signals in your body, effectively numbing the area where it is administered. This article will explore the mechanism of action, uses, and effects of ropivacaine powder in the human body.
What are the main uses of Ropivacaine Powder in medical procedures?
Ropivacaine powder is widely used in various medical procedures due to its effectiveness and relatively long duration of action. Some of the primary applications include:
- Surgical anesthesia: Ropivacaine is commonly used for local and regional anesthesia during surgical procedures. It can be administered through epidural injection, peripheral nerve blocks, or infiltration into the surgical site. This allows surgeons to perform operations while the patient remains conscious but pain-free in the targeted area.
- Postoperative pain management: After surgery, ropivacaine can be used to provide extended pain relief. This is often achieved through continuous infusion or patient-controlled analgesia systems, allowing for better pain control and reduced need for systemic opioids.
- Obstetric procedures: Ropivacaine is frequently used in obstetrics for labor analgesia and cesarean sections. Its properties make it particularly suitable for these procedures, as it provides effective pain relief while minimizing motor blockade, allowing mothers to remain more mobile during labor.
- Chronic pain management: In some cases, ropivacaine may be used in the management of chronic pain conditions. This can include nerve blocks for conditions such as complex regional pain syndrome or chronic back pain.
- Dental procedures: Ropivacaine can be used in dental surgeries and procedures to provide local anesthesia, ensuring patient comfort during potentially painful interventions.
The versatility of ropivacaine powder in medical procedures stems from its favorable pharmacological profile. It provides effective sensory blockade while causing less intense motor blockade compared to some other local anesthetics. This characteristic allows for better mobility and earlier recovery in many cases.
Moreover, ropivacaine has a longer duration of action compared to lidocaine, another commonly used local anesthetic. This prolonged effect can be beneficial in many surgical and pain management scenarios, reducing the need for repeated administrations or additional pain medications.
The use of ropivacaine in medical procedures also contributes to enhanced recovery after surgery (ERAS) protocols. By providing effective local anesthesia and post-operative pain control, ropivacaine can help reduce the overall stress response to surgery, potentially leading to faster recovery times and shorter hospital stays.
How long does the numbing effect of Ropivacaine Powder typically last?
The duration of the numbing effect produced by ropivacaine powder can vary depending on several factors, including the concentration used, the method of administration, and individual patient characteristics. Generally, ropivacaine provides a longer-lasting anesthetic effect compared to many other local anesthetics.

Typical durations of action for ropivacaine include:
- Peripheral nerve blocks: The numbing effect can last anywhere from 5 to 18 hours, with an average duration of about 9-14 hours. This extended duration makes ropivacaine particularly useful for postoperative pain management.
- Epidural anesthesia: When used for epidural anesthesia, the effect of ropivacaine can last between 4 to 6 hours, although this can be extended with continuous infusion techniques.
- Local infiltration: When injected directly into tissues, the numbing effect of ropivacaine typically lasts for 2 to 6 hours, depending on the concentration used and the specific site of injection.
The prolonged duration of action of ropivacaine is one of its key advantages in clinical practice. This extended effect allows for better pain control during and after surgical procedures, potentially reducing the need for systemic analgesics and their associated side effects.
It's important to note that the onset of action for ropivacaine is slightly slower compared to some other local anesthetics like lidocaine. The full anesthetic effect typically develops within 10 to 20 minutes after administration. This slightly delayed onset is often balanced by the longer duration of action.
Factors that can influence the duration of ropivacaine's numbing effect include:
- Concentration: Higher concentrations of ropivacaine generally result in a longer duration of action.
- Addition of vasoconstrictors: The addition of epinephrine can prolong the duration of action by reducing systemic absorption.
- Patient factors: Individual variations in metabolism, body composition, and the presence of certain medical conditions can affect how long the numbing effect lasts.
- Site of administration: The specific location where ropivacaine is administered can influence its duration of action due to differences in local blood flow and tissue composition.
Understanding the typical duration of ropivacaine's numbing effect is crucial for healthcare providers in planning pain management strategies and ensuring patient comfort throughout medical procedures and recovery periods.
Can Ropivacaine Powder be used for nerve blocks, and if so, how effective is it?
Yes, ropivacaine powder can be used for nerve blocks, and it is indeed one of its primary applications in clinical practice. Nerve blocks involve injecting local anesthetic near specific nerves or nerve bundles to interrupt pain signals from a particular area of the body. Ropivacaine has proven to be highly effective for this purpose, offering several advantages over other local anesthetics.
The effectiveness of ropivacaine for nerve blocks can be attributed to several factors:
- Potency: Ropivacaine is a potent local anesthetic, capable of providing effective sensory blockade at relatively low concentrations. This allows for efficient pain control while minimizing the risk of systemic toxicity.
- Duration of action: As mentioned earlier, ropivacaine offers a longer duration of action compared to many other local anesthetics. For nerve blocks, this can translate to prolonged pain relief, often lasting 9-14 hours or more, depending on the specific technique and concentration used.
- Differential blockade: One of the unique properties of ropivacaine is its ability to produce differential sensory-motor blockade. At lower concentrations, it tends to block sensory nerves more than motor nerves. This can be advantageous in situations where pain control is desired without complete motor paralysis.
- Safety profile: Ropivacaine has a favorable safety profile compared to some other local anesthetics, particularly regarding cardiac and central nervous system toxicity. This makes it a preferred choice for many clinicians, especially when larger volumes of local anesthetic are required.
The effectiveness of ropivacaine in nerve blocks has been demonstrated in numerous clinical studies across various surgical specialties. Some notable applications include:
- Brachial plexus blocks: For upper limb surgeries, ropivacaine has shown excellent efficacy in providing anesthesia and postoperative analgesia. Studies have reported successful blocks with durations of analgesia extending beyond 12 hours.
- Femoral and sciatic nerve blocks: In lower limb surgeries, ropivacaine-based nerve blocks have been shown to provide effective pain control, often reducing or eliminating the need for opioid analgesics in the immediate postoperative period.
- Thoracic paravertebral blocks: For chest wall procedures and breast surgeries, ropivacaine has demonstrated high success rates in achieving adequate anesthesia and prolonged postoperative analgesia.
- Epidural anesthesia and analgesia: While not a peripheral nerve block, epidural administration of ropivacaine is widely used in obstetrics and major abdominal or lower limb surgeries, providing effective pain control with the advantage of a motor-sparing effect at lower concentrations.
The effectiveness of ropivacaine in nerve blocks is further enhanced by modern techniques such as ultrasound-guided administration. This allows for precise localization of nerves, potentially improving block success rates and reducing the volume of local anesthetic required.
It's worth noting that while ropivacaine is highly effective for nerve blocks, its use should always be tailored to the specific patient and procedure. Factors such as the patient's age, weight, medical history, and the nature of the surgery all play a role in determining the optimal approach to regional anesthesia.
In conclusion, ropivacaine powder has proven to be a highly effective agent for nerve blocks across a wide range of clinical scenarios. Its long duration of action, differential blockade properties, and favorable safety profile make it a valuable tool in the anesthesiologist's armamentarium for providing effective pain control and enhancing patient outcomes.
If you are also interested in this product and want to know more product details, or want to know about other related products, please feel free to contact sasha_slsbio@aliyun.com.
References:
- Kuthiala G, Chaudhary G. Ropivacaine: A review of its pharmacology and clinical use. Indian J Anaesth. 2011;55(2):104-110.
- Casati A, Putzu M. Bupivacaine, levobupivacaine and ropivacaine: are they clinically different? Best Pract Res Clin Anaesthesiol. 2005;19(2):247-268.
- Feldman HS, Covino BG. Comparative motor-blocking effects of bupivacaine and ropivacaine, a new amino amide local anesthetic, in the rat and dog. Anesth Analg. 1988;67(11):1047-1052.
- Markham A, Faulds D. Ropivacaine. A review of its pharmacology and therapeutic use in regional anaesthesia. Drugs. 1996;52(3):429-449.
- McClure JH. Ropivacaine. Br J Anaesth. 1996;76(2):300-307.
- Scott DB, Lee A, Fagan D, Bowler GM, Bloomfield P, Lundh R. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesth Analg. 1989;69(5):563-569.
- Fanelli G, Casati A, Beccaria P, et al. A double-blind comparison of ropivacaine, bupivacaine, and mepivacaine during sciatic and femoral nerve blockade. Anesth Analg. 1998;87(3):597-600.
- Klein SM, Greengrass RA, Steele SM, et al. A comparison of 0.5% bupivacaine, 0.5% ropivacaine, and 0.75% ropivacaine for interscalene brachial plexus block. Anesth Analg. 1998;87(6):1316-1319.
- Brockway MS, Bannister J, McClure JH, McKeown D, Wildsmith JA. Comparison of extradural ropivacaine and bupivacaine. Br J Anaesth. 1991;66(1):31-37.
- Chelly JE, Ghisi D, Fanelli A. Continuous peripheral nerve blocks in acute pain management. Br J Anaesth. 2010;105 Suppl 1:i86-96.

